“`html
Effective Ways to Get Rid of Fungal Acne in 2025
Fungal acne can be a stubborn and frustrating skin condition that many people struggle with. In this article, we will explore effective ways to tackle fungal acne, providing insights into its causes, symptoms, and the best treatments available in 2025. If you’re looking for ways to enhance your skincare routine with an emphasis on the right products and lifestyle changes, you’ve come to the right place.
Understanding Fungal Acne Causes and Symptoms
Fungal acne, often confused with regular acne, is caused by an overgrowth of yeast on the skin, specifically Malassezia. This condition can occur due to various factors, including oily skin, hormonal changes, and even certain diets. The symptoms of fungal acne may include itchy, red, and inflamed bumps that resemble traditional acne but often appear in clusters. Understanding how to identify fungal acne is crucial for effective treatment.
How to Identify Fungal Acne
Recognizing fungal acne can be challenging, especially since its appearance is similar to that of regular acne. Typically, fungal acne manifests as small red or skin-colored bumps, primarily on the forehead, chest, and back. These bumps do not respond well to conventional acne treatments like benzoyl peroxide. If you notice a persistent rash that doesn’t improve with standard acne treatments, you may be dealing with fungal acne. Consulting with a dermatologist can help confirm the diagnosis.
Common Fungal Acne Triggers
Several factors can contribute to the development of fungal acne. One common trigger is excessive moisture and humidity, which promotes yeast growth on the skin. Additionally, diets high in sugar and refined carbohydrates can exacerbate fungal acne, as they feed the yeast. It’s essential to identify your personal triggers as part of managing fungal acne effectively. Keeping a skincare journal may help track what factors seem to worsen your condition.
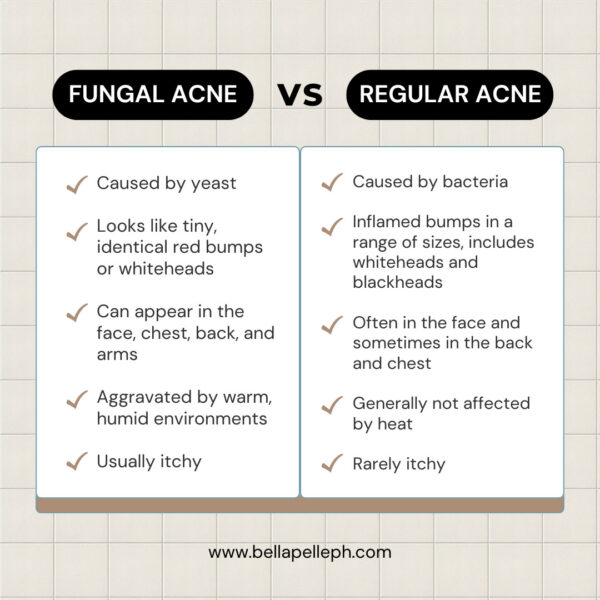
Fungal Acne vs Regular Acne
Understanding the difference between fungal acne and regular acne is vital for choosing the correct treatment approach. While traditional acne is often caused by blocked pores and excess oil production, fungal acne occurs due to an overgrowth of yeast. Regular acne responds well to salicylic acid and benzoyl peroxide, whereas antifungal treatments, like **antifungal creams for acne**, are necessary for fungal acne. Consulting a dermatology specialist can clarify your diagnosis and direct appropriate fungal acne treatment options.
Fungal Acne Treatment Options
When it comes to treating fungal acne, various options can be highly effective. Antifungal creams and over-the-counter products designed specifically for fungal infections are powerful tools in managing this skin condition. Moreover, formulating a dedicated skincare routine that incorporates antifungal ingredients is vital for long-term success.
Using Topical Treatments for Fungal Acne
Topical treatments for fungal acne are foundational in managing symptoms. Look for over-the-counter antifungal creams containing ingredients like clotrimazole or miconazole. These ingredients help to eliminate the yeast responsible for fungal acne. Regular application of these creams, alongside a consistent cleansing routine, can significantly reduce fungal acne breakout occurrences.
Best Products for Fungal Acne
Choosing the right products is crucial when managing fungal acne. Products containing **natural antifungal agents** like tea tree oil and **probiotics** can support skin health and balance the microbiome. Moreover, it’s essential to avoid heavy moisturizers and oil-based products, as they may contribute to fungal growth. Instead, look for lightweight, water-based moisturizers labeled safe for fungal acne—which often include ingredients like hyaluronic acid.
Fungal Acne Home Remedies
Natural remedies for fungal acne can complement medical treatments. Ingredients like **coconut oil** have antifungal properties and may alleviate symptoms. A simple home remedy involves mixing diluted apple cider vinegar with water and applying it as a toner. Remember to perform a patch test first to ensure your skin doesn’t react negatively. Even with home remedies, consider consulting a dermatologist for tailored advice.
Fungal Acne Skincare Routine
Developing a proper skincare routine can significantly impact the management of fungal acne. This routine should focus on gentle cleansing, applying antifungal treatments, and moisturizing with safe ingredients only. Keeping it simple can help minimize the chances of irritation and breakouts.
Creating a Gentle Cleansing Routine
A well-structured cleansing routine is essential for fungal acne management. Start with a **gentle cleanser free from harsh chemicals** and fragrances, as these can irritate the skin. Look for **antifungal face washes** that include ingredients intended to neutralize excess yeast. Cleanse twice daily and follow up with an appropriate antifungal treatment to enhance effectiveness.
Moisturizing Tips for Fungal Acne
Moisturizing can be tricky with fungal acne. A **fungal acne safe moisturizer** should be lightweight and non-comedogenic, containing ingredients that offer hydration without promoting yeast growth. Incorporating moisturizers with niacinamide can provide anti-inflammatory benefits and strengthen the skin barrier, helping to prevent further breakouts.
Fungal Acne Prevention Tips
Preventing fungal acne is often easier than managing an outbreak. To prevent fungal growth, focus on lifestyle changes, such as managing sweat, maintaining a balanced diet, and using breathable fabrics. Using antifungal powder on skin folds and areas prone to moisture can further help in moisture control. Regularly washing linens and wearing clean clothes can also decrease your chances of recurrent fungal acne.
Key Takeaways
- Identify fungal acne through its unique symptoms and triggers.
- Utilize effective antifungal treatments and choose skincare products carefully.
- Establish a consistent skincare routine focused on gentle cleansing and appropriate moisturization.
- Implement dietary and lifestyle modifications to prevent future outbreaks.
FAQ
1. How long does it typically take for fungal acne to heal?
The healing time for fungal acne varies depending on individual skin responses to treatment but generally ranges from a few weeks to several months. Regular use of antifungal treatments and adherence to a dedicated skincare routine can speed up the process.
2. Are there specific diets that can help with fungal acne?
Diets low in sugar and refined carbohydrates are often recommended for individuals with fungal acne. These dietary modifications help manage blood sugar levels and minimize yeast growth, potentially reducing outbreaks.
3. Can I use regular acne treatments on fungal acne?
Conventional acne treatments like benzoyl peroxide are usually ineffective against fungal acne, as they don’t target yeast. It is crucial to use *antifungal creams for acne* or specialized products instead.
4. Can stress contribute to fungal acne flare-ups?
Yes, stress can adversely impact your skin and contribute to acne flare-ups, including fungal acne. Stress management techniques, such as yoga, meditation, or regular exercise, can support overall skin health.
5. When should I consider seeing a dermatologist for fungal acne?
If you find that over-the-counter treatments are ineffective, or if your symptoms worsen, it is advisable to consult a dermatologist. A specialist can provide tailored treatments and possibly prescribe systemic antifungals.

“`
